I’m really thrilled to be writing this post because it seems I’ve finally truly gotten rid of a chronic heel/Achilles/plantar fasciitis issue that has been with me for a long time. (I’ve said this before and I’ve been wrong, but for the record I’ve been running a lot and my heel hasn’t felt this good for this long in years.)
This thing has been with me for maybe three years. It’s never been enough to really knock me out. It didn’t derail me from my first marathon and subsequent 10-milers and half-marathons. However, several weeks ago I did a long trail run and it felt like a nail had been driven into my heel. I figured it was time to sort this out. The solution has been a mix of biomechanical and running technique adjustments, and a deeper understanding of pain science.
Before I met with anyone I put a green Superfeet insert into my shoes. I’m a minimalist shoe advocate. I don’t want to rely on a crutch but I’m also very much willing to do whatever is appropriate to solve a problem. A lot of what I’ve read for addressing heel and Achilles problems suggests putting some sort of insert into a shoe. The idea here was to unload some of the muscles and structures that hold up the foot, including the Achilles. I’m still using the inserts on a lot of my runs but I rarely wear them at work and I do some of my runs with without the insert.
I next met with a couple of guys with a lot of great knowledge and experience. Mike Terborg and Nick Studholme were both very instrumental in my progress. Mike is a performance and injury recovery specialist in Boulder and Nick runs Studholme Chiropractic. Mike is heavily influenced through John Hardy and the principles of FASTER Global which teaches a process of biomechanical reasoning. Nick studied under the innovative physical therapist Gary Gray. Both guys speak much the same language when it comes to movement and movement analysis.
They both have tremendous ability to explain what they see and communicate the changes they thought I should make. They both used a fantastic and powerful video program called Spark Motion which was created by Nick and a group of other guys. This was just an amazing way to record and analyze movement. Spark is a great tool that I need to look into.
The visit with Mike Terborg: Running adjustments
I first visited with Mike in Boulder a few weeks ago. We spent a couple of hours looking at how I moved. The major issue we found was prolonged eversion of my left foot. The foot stayed in contact with the ground for what seemed a long time. Mike explains his observations and thought process:
“Adhering to the Biopsychosocial or BPS model of pain (vs the Postural-Structural-Biomechanical model), we couldn’t say for sure what was causing the pain other than it could be a combination of things including but not limited to biomechanics. You had chronic pain of the plantar fascia, like to run, and wanted to be able to run more without aggravating this injury so we needed to look at your physiological skills and tendencies relative to gait. We cannot say for sure that eversion and dorsiflexion of the subtalar joint caused the injury (because these are natural motions of subtalar joint and thus normal motions for the PF to decelerate), but we can deduce that less loading of the plantar fascia (less dorsi/eversion) might be helpful in reducing the amount of stress on the PF during running. Our hope was that less stress/load during gait may allow you to run pain free for longer. In sum, we can say for sure that we crossed some type of stress threshold (bio, psycho and or social), so we wanted to ask your body what happened if we backed off on the biomechanical load to the pissed off tissue.
“Your ranges and sequencing in the breakout evaluation all looked good, so we went straight to your running technique. Using Spark Motion for gait analysis, we deduced that it was possible for you to run in a way that reduced the stress to your PF and apparently that helped. The drills were all part of a progression to not only teach your body the skills and sequence of a more rapid gait but to train your ability to sustain that gait for longer periods of time (strength endurance of a skill). Nothing fancy, just following biomechanical reasoning to look for clues and strategies.”
I really like Mike’s explanation of the process. He puts his explanation in a very honest way. In saying that we don’t know for certain why the pain is there, nor do we understand exactly how or why it might go away, he reflects the current cutting edge of pain science which reveals that pain is in many ways a baffling mystery.
He directed me to several exercise progressions of which here are three:
We changed my running gait along these lines:
- Put less pressure through the heel into the ground. Let the heel touch the ground but only lightly.
- Quicken the stride so the foot stays in contact with the ground for less time.
- Swing the right leg through faster to facilitate less time on the ground of the left foot.
- Run with a metronome set somewhere between 170-190 bpm. This quickens the stride rate. Experiment.
The resulting new gait felt like I was some sort of prancing fool–La la la la laaaa!!!–dancing through the daisies. Fortunately the video Mike shot of me indicated that in fact I just looked like I was running with a quicker step. (I could in fact go running in public this way.) Finally, Mike also suggested I visit with Nick so I did.
Analysis from Nick Studholme & fine tuning the lower leg
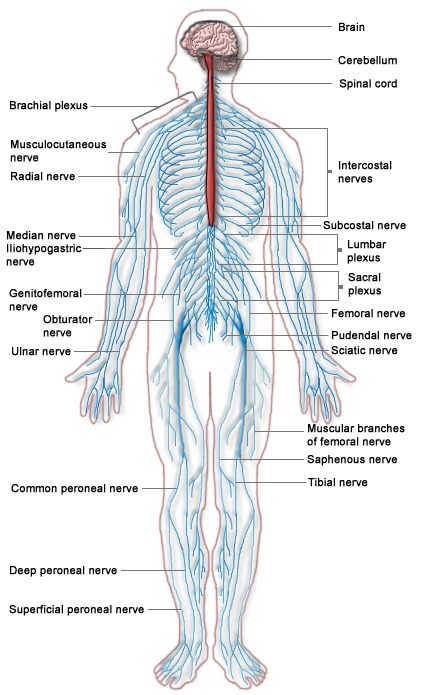
Nick put me through a muscle testing process and winnowed out some weak and unstable muscles in my lower leg. Specifically, big toe muscles known as flexor hallucis longus, and flexor hallucis brevis weren’t working up to par. The fibularis muscles (aka peroneals) were also a bit off line.
Taken together, when these muscles work they create and control plantar flexion and inversion of the foot as in the push-off of running or walking, and they create/control dorsiflexion and eversion of the foot as when the foot hits the ground.
Of great importance is the ability to anchor the big toe to the ground while the body passes over the foot. I was missing the mark. Nick taped my foot in a way to help facilitate this anchoring and he showed me several exercises to help me feel, create and control better big toe function while running. These exercises were similar in nature to what Mike showed me.
It’s several weeks later and what are the results? The heel and Achilles quickly started feeling better. I did a series of short interval type runs. The quicker pace (around 175-180 bpm) was challenging at first. I didn’t want to become exhausted while running and lose the technique, thus I only ran 1 or 2 minutes at a time. and walked in between. (Running with my dog tends to be a good way to break up the running with walking.)
Some discomfort remained for a couple of weeks in a stubborn way. It wasn’t terrible but it was hanging around like it was ready to pounce. I was worried that there was something we might be missing. This last bit of hanging-around heel trouble would be gone within 48 hrs after I reviewed the current ideas on pain and the brain. I’ll discuss that in the next post.