No gym? No problem. Get Strong at Home.
StandardHere are 13 exercises to build strength and improve your running form right in your living room or yard. Check out my latest article for Podium Runner: No gym? No Problem. Get Strong at Home. Here’s one exercise, the improvised squat:
3D Ankle, Hip, & Spine Mobility Exercises for Runners
Standard
Running occurs in three planes: sagittal (front/back), frontal (side-to-side), and transverse (left/right rotation.) Efficient, healthy running happens when your joints are able to move freely through these three planes. For runners, full-range movement at the ankles, hips, and thoracic spine (t-spine) is crucial. Unfortunately, our modern lifestyle may be an impediment to good running. Sitting, hunched forward for work and travel promotes rigid, poorly moving joints.
Running requires you to generate force for propulsion and absorb impact forces. Optimally, those forces are distributed efficiently through all of your joints, muscles, connective tissue, and bones. If a joint is restricted, then forces are distributed inefficiently and certain tissues may receive more stress than they can withstand. The consequences of poor joint mobility may include tendinopathies, and pain in your knees, hips, low-back, shoulders, and/or neck. You can guard against these problems by addressing mobility in your ankles, hips, and trunk.
The following exercises are dynamic drills, not static stretches. You’ll drive in and out of the position of stretch. Hold the stretch no more than about a second.
You can read the rest of my latest article at Podium Runner.
Got Pain? Don’t Stretch, Strengthen.
Standard
If you’re like many runners, stretching is your first course of action when you feel pain. Sore Achilles tendon? Stretch the calf. Sore knee? Stretch the quads or the IT band.
The problem is, tight muscles are rarely the root cause of pain, so stretching rarely solves the problem. A better solution for chronic, training-related pains and injuries—one with more evidence behind it—is strength training.
Read the rest of the article, my latest for PodiumRunner.com.
Be Patient. Don’t Rush. Lift Better.
Standard
Explosive lifts such as the barbell power clean and the kettlebell swing should happen fast. Why else would they be called “explosive?” Creeping slowly through the lift, muscling the weight, and being overly cautious won’t work. You must create great momentum to swing and clean correctly. Cleans and swings SHOULD NOT be rushed though. Both lifts require sound technique which means moving the right way at the right time. If you’re impatient and you rush these lifts then the results will be less than optimal. You must be patient.
the barbell clean
A successful barbell power clean requires moving upward explosively then moving quickly underneath the bar to catch it. Recently a client was impatient to get under the bar. Her technique wasn’t terrible but clearly something was off. We went through the lift in super-slow motion without a bar. I coached her to be patient at the apex of the lift and spend an exaggerated amount of time up there before dropping under the bar. It instantly improved her clean. I saw it and she felt it.
the kettlebell swing
With the kettlebell swing, I see people rushing at both at the top and the bottom of the lift. They cut off the arc of the swing and try to force the bell up or down. My coaching strategy is this:
- On the upswing: Be patient. Stand tall. Allow the bell to rise and float at the top.
- On the downswing: Be patient. Relax and go with the momentum of the bell, allowing it to swing where it wants to go.
exaggeration
In both examples, the client’s technique is wrong but it feels normal. Thus, the correct technique should actually strange. It should actually feel exaggerated. The client should feel like he or she is spending too much time at the top of the clean or at the top and bottom of the swing.
patience elsewhere
Getting fit, strong, and healthy takes time. It never happens as fast as you want. Patience and persistence aren’t exciting words. Those concepts don’t spark fads or sell books. Brad Stulberg offers this pertinent take:
Lasting change almost always happens incrementally and over time—the result of repeated bouts of consistent effort. Don’t get fooled by radical, overnight success stories. Most people who go for broke end up broke. It’s just that those stories don’t get told.
— Brad Stulberg (@BStulberg) January 8, 2020
Pain: What you should know
Standard
I’ve become a fan of the Stronger by Science podcast. The hosts, Eric Trexler and Greg Nuckols are a pro natural bodybuilder and an accomplished powerlifter, respectively. They both hold science-related degrees and they’re trained in research and statistics. They translate research into meaningful information. They do a good job of discussing the weaknesses and strengths of various studies and they debunk a lot of fitness-related nonsense, a lot of which is floating around.
I recently listened to episode 22 in which they interview Dr. Michael Ray, DC, a contributor to Barbell Medicine.com. The topic was pain, a subject I find fascinating. It’s a good interview, one that gave me a new view of a subject I’ve studied for years. Following the interview, I went to BarbellMedicine.com and found an excellent article titled Pain in Training: What do? (I think it was probably intended to be titled Pain in Training: What to do? but I’m not sure.) If you’re a fitness or rehab professional or if you’re an athlete or fitness enthusiast who’s in pain then you should read it. Learning about pain will help you overcome it. Here are the key points I took from the article:
- Hurt does not equal harm. You can have pain without damage and damage without pain. The intensity of pain is often a poor reflection of the magnitude of damage—if there’s any damage at all.
- Trainers, coaches, and therapists should not create fear of movement. The article states, “So it is reasonable to coach a particular movement style for the purposes of performance and efficiency, but we deliberately avoid pairing our movement cues with unnecessary messages (either overt or subliminal) of danger or threat. In the same way, we criticize irresponsible healthcare professionals who warn those with back pain that ‘One wrong move and you’re paralyzed,’ we similarly criticize coaches who perpetuate the belief that ‘If you let your technique slip, you’ll get injured,’ since these ideas induce unnecessary hyper-vigilance and threat around exercise.”
- Rest rarely works. The article says, “One approach we typically do NOT recommend for most routine aches and pains in the gym is absolute rest.” And, “Additionally, we have evidence in several contexts that absolute rest often results in either no improvement (e.g. in tendinopathy) or worse outcomes (e.g., in low back pain).”
- Find an entry point to exercise. This stuck in my mind. It got me thinking. Here, we want to “find a type and dose of exercise stimulus that results in either improved symptoms or stable symptoms over the subsequent 24-48 hours after training. A marked increase in symptoms during or after training reflects a dose of stimulus that is likely too high in terms of intensity, volume, or both.”
Variables that may be manipulated include load, range of motion, tempo (pace the lifter uses while lifting), or exercise variation. I haven’t experimented with tempo, or speed of movement. I’ll will have my clients moving with different tempos in the near future.
I’ve studied pain for years and I feel like I have a solid grasp of how it works and what it means, but it’s always useful to revisit this information. I always learn something new. Read the entire article to learn a lot more.
Glutes: Linear and Rotational Training
Standard
I’ve had a lightbulb moment thanks to an Instagram post by Brett “the Glute Guy” Contreras, PhD. (I wish I’d saved the post. Now I can’t find it… Oh well.) He described training the glutes in both a linear and rotational fashion. This makes sense when considering the alignment of the muscle fibers of the glute muscles with the glute max being the best example. The fibers are diagonal which means they can exert force both both in a straight line and in rotation.
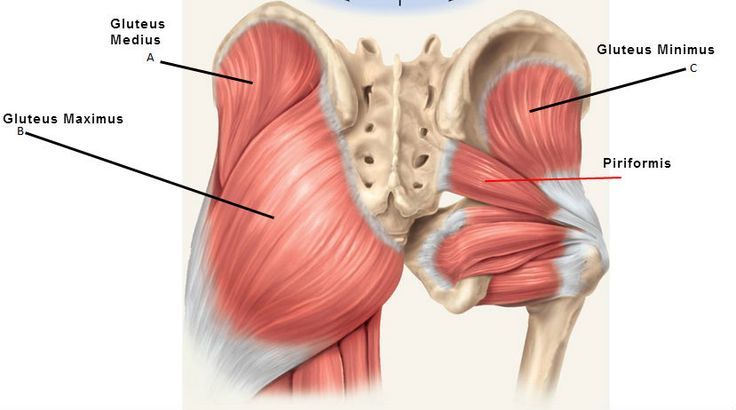
The gluteus maximus fibers facilitate both sagittal plane and transverse plane movement.
I’ve long used exercises that train the glutes linearly: squats, lunges, and deadlifts for example. And now I recognize that I’ve only scratched the surface or paid lip service to the rotational ability of the glutes. I’ve gained a new appreciation for some exercises that long avoided, such as the clamshell.
I’ve been doing more clamshells in my own workouts to help address some of the faulty foot mechanics that led to some recent toe pain. The glutes play a powerful role in controlling how the feet move and I believe clamshells and other rotational glute exercises have helped me.
Linear exercises
- Deadlift, 1- and 2-legged
- Squats, 1- and 2-legged (1-legged squat)
- Romanian deadlift, 1- and 2-legged (Video 5 is a 1-leg RDL)
- Kettlebell swings (Video 8)
- Bridges
- Barbell hip thrusts (Video 1)
- Most lunges and split-squats
- Forward step-ups
- Good mornings (video 6)
- Single-leg tube squat with the tube attached straight ahead
- Sprints
Rotational exercises
- Clamshells
- Lateral band walks
- Hip airplanes
- Lunges with rotation
- Single-leg tube rotation
Anti-rotation exercises
These exercises impose a load on the body that will try to rotate you. Your job is to resist the rotational forces. These are really whole-body exercises but the glutes are definitely involved.
- Anti-rotation squat
- Anti-rotation split squat (video 3)
- Single-leg tube squat with the tube attached to the side
- Offset Romanian deadlifts (video 4)
Exercise wisdom
In almost 20 years of training, I’ve thrown many babies out with some bathwater. I’ve fallen for dogma and rejected certain exercises because I thought they weren’t “functional” or had no carryover to life outside the gym. The clamshell exercise is one example. Who needs to have strong hips while lying down sideways? What use is that, especially to athletes?
It’s a relief to discover that very smart exercise professionals have had a similar experience. Physiotherpist, chiropractor, and pain expert Greg Lehman said this about the clamshell as it pertained to runners:
“I used to abhor the clamshell. Then I started testing more runners with the clamshell. A number who tested strong in many positions would tremble during the clamshell. Crazy, they had a lovely one leg squat, strong hip abduction but had trouble with 10 or 15 clamshells. What does that tell me? Such a massive deficit in function. Would you suggest clamshells here or something to address that specific movement? This seems like a case where I would suggest clamshells. If a runner can’t do them I would want to address that deficit.
“But, do I want to see every runner doing them as part of a ‘functional’ program. Of course not. They suck for that. This is a case where the exercise prescription is ‘functional’ because it addresses a specific limitation in a specific runner.”
The clamshell is also recommended by physical therapist, and running/cycling coach Jay Dicharry.
I’ve returned to various exercises with a new appreciation. I hope that as I age and gain experience that I also gain wisdom. I must remember to maintain some skepticism about just about everything. At the same time, I should be willing to revisit what I think I know and reevaluate my thoughts.
Injury, A Sick Dog, & Getting Through a Bad Experience
StandardI call it the 24-hour rule… which is that after a big success or a bad failure, give yourself 24–48 hours to celebrate the success or grieve the defeat. But then, get back to doing the work itself.
The longer that you stew in a loss or ride the dopamine high of a win, the more you are becoming addicted to that. Whereas if you go back to doing the work itself, it’s a very embodied way of reminding yourself that, Hey, what I really like is the activity, not all the fortune, fame, external validation from the activity.”
That is sage advice from Brad Stulberg, author of Peak Performance and The Passion Paradox. I’ll return to it soon.
The past couple of weeks have been full of emotional highs and lows, frustration, elation, anger, and gratitude. I’m pleased that I came out feeling good in the end despite some disappointment. The big picture is this: I was unable to run the Grand Traverse Run on 8/31.
One week out – Toe pain
Metatarsalgia, aka ball-of-foot pain, roared to life exactly one week plus one day prior to the race. I’d had this in the past but hadn’t felt it in over a year. It was during an interval run. It wasn’t anything out of the ordinary. The pain typically subsides quickly but this time it didn’t. Anger/panic set in.
The 40.7 miles of high mountain running was already intimidating. My prior long race was a trail marathon at 26.2 mi. This was almost 15 mi. longer and it topped out at 12,000 ft. of elevation. I was staring into the unknown. Now, on top of it, a true painful problem was ominous. I was genuinely worried, not just nervous. This was the 2nd year in a row that an injury threatened to derail this deeply meaningful project. All the hard work I’d put in might be for nothing.
I scheduled time with a physical therapist. She assessed some surprising weakness in my hip abductors, specifically the glute medius. That muscle contributes significantly to foot posture. Her assessment gave me valuable information on how to address a weakness in my running but that solution would take time, weeks or months. I had to race in just a few days.
I also met with Dr. Nick Studholme at Studholme Chiropractic in Denver. He’s helped me in the past. He taped my feet to unload the area under the 2nd toe. This wasn’t a fix, but something to help me get through the race. Unfortunately, a short test run the day after the taping wasn’t good. My foot still hurt a lot. I was despondent.
Finally, I had a cortisone shot. I am not a fan of cortisone. The long-term effects of too much cortisone aren’t good. Cortisone is definitely not a fix, but rather a powerful band-aid. For my purposes in this situation, cortisone was exactly what I needed. It was time to run. I would deal with the injury later.
Fast-forward to the day before the race: I felt good. I had no foot pain. We were in Crested Butte and I felt positive. In the course of a week, I’d gone from despondent to optimistic.
A sick dog, a super wife, & damn you Google
Race time was 6 am. I would get up at 4:15 am to get ready. My wife and our dog, Diva, would make the 3+ hour drive to Aspen and meet me at the finish. We all needed rest.
Diva started a hacking cough/dry heave Friday afternoon as we checked into our hotel. We didn’t know why. Dogs do this some time. She gobbled grass. Lots of it. This also happens sometimes. She finally threw up. Typically that’s the end of the story but not this time. She kept hacking. Constantly. We figured it would stop any time. It didn’t. This kept on into the night. Diva paced and coughed, coughed and paced. No one slept.
Finally, around 11 pm, my wife got online and found two 24 hr vets in Gunnison, about 30 miles away. She would take our dog and let me sleep. A super wife! Time ticked away rapidly. Race time was racing my way. I slept.
I woke up, middle of the night. They hadn’t returned They came in a little while later. Both 24-hour vets were closed. Google lied! Our dog was still sick but not worse. The prospect of racing was slipping away. My wife was seriously sleep deprived. Driving would be unsafe. We thought our dog probably needed a vet visit. I hadn’t had much more sleep. The reality of the situation dawned and it was clear I couldn’t race. I didn’t have words for this defeat. Rotten, bloody hell… Nothing else to do.
We headed home. Diva continued to improve. My wife and I had good conversation on the way back. No strife.
The rollercoaster continues
I’d built all this fitness so why waste it? I registered for the Sage Burner 55k in Gunnison at the end of October. We’ve only passed through Gunnison and never spent time there. Though this race didn’t have the epic appeal of the Grand Traverse, I was very happy and excited to run it and to spend time in Gunnison. More despair was around the corner though.
Sunday, the day after the race, I ran with the Denver Trail Runners at Gorgeous Kenosha Pass. It was a perfect, bright, cool day. No crowds on the trail. Three miles in the toe pain returns, just like before. I’m crushed, furious. No sense in running further, I’ll just hurt it more, I turned around and headed back to the trailhead.
On the return, I started to play with how my foot hits the ground and how I push off. I biased heavily to the outside of the foot. Not that I’m walked with my foot completely inverted but I deliberately created more pressure and more pushed through the outside of the foot. The pain decreased. I started jogging with this outside bias. Pain decreased more. I ran back to the parking area with virtually no pain. I turned around and ran back out to meet the group on the return. I finished having run just shy of 13 miles. Greatness! This was the polar opposite of missing the race. Another occasion where words don’t work to describe the feelings! Spectacular! I felt like this:

WAAAHOOOO!
Gratitude & no whining
Hard times and defeat always provide a learning opportunity. I can’t decide how I feel but I can decide how I react to those feelings. The pain of missing this race for the 2nd year in a row was powerful. Made me sick to my stomach. How could I react? Pout, gripe, and rage? Did my wife need to hear repeatedly how bad I felt, even though she already knew? Would complaining change the past? Nonsense nonsense nonsense! Complaining about something over which I have no control is a waste of energy and it may even be bad for my mental health. It’s bulls%it, to put it another way.
I did grieve the race though. I spent about 24 hrs feeling the disappointment. I felt sad and incredibly frustrated. There was no use in ignoring those feelings. But griping and whining had no place in the process. It was time to get back to work in preparation for the Sage Burner. My coach, Andrew Simmons of Lifelong Endurance has been a tremendous help. He’ll be guiding me for another couple of months.
There was a time in my life when I felt like my life was lacking a lot of things. I fixated on my failings and what I didn’t have. That wasn’t useful. Now I try to be grateful for the multitude of good people and things in my life. Specifically, in this case, I was and am grateful for the following: grateful that Diva got well; grateful for my wife who supported my efforts; hugely grateful for that good Sunday trail run during which my foot felt bad and then good; grateful for my friends, clients, and family who donated to NRDC (You can still donate btw!); grateful for being a trail runner with the chance to do something few people will ever imagine.
Everything isn’t always perfect, but most things are pretty good.
8 Ways to Improve Your Running Posture
Standard
The position of the trunk and hips is critical for efficient, healthy running.
I’m pleased to share 8 Ways to Improve Your Running Posture, my latest article in Podium Runner. Running posture is vital for effective, healthy running. This article teaches you to mobilize joints that may inhibit good posture, and how to strengthen key muscles that reinforce good posture and make for stronger running. Here’s an excerpt:
Running is clearly a lower-body dominant activity. That said, you should understand that your body is an interconnected system more than it is a collection of parts. Running involves your entire body, from head to toes. That means your running posture—the position in which you hold your hips and spine while running—matters.
Optimal running posture is:
- Comfortable: Able to run hard without pain.
- Efficient: Use the least energy required for a given pace.
- Minimally stressful: Forces generated by impact and propulsion are distributed evenly throughout your bones, muscles, and connective tissues.
Read the rest of the article, 8 Ways to Improve Your Running Posture.
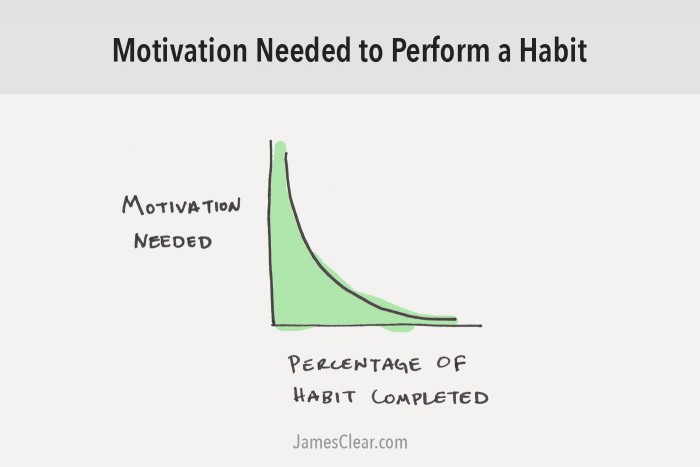
Which Comes First, Motivation or Action?
Standard… this is basically Newton’s First Law applied to habit formation: Objects in motion tend to stay in motion. Once a task has begun, it is easier to continue moving it forward.
– James Clear
An important task stares us in the face. We vegetate and pray for supernatural intervention to either complete the task or remove it from existence. We know the task is important to our health and wellbeing. But our emotions undermine us and we avoid the gym, delay meeting with a financial planner, or avoid scheduling an appointment with a doctor or mental health counselor. Or we just hope the lawn will mow itself.
The search for motivation is common to everyone. I’ve spent weeks at a time not posing on this blog but knowing that if I want to be a writer then I must write. The dread and self-loathing builds… I may long to improve my physique and drop some body fat, yet I eat the same: I love a cocktail and some dessert—and those flabby trouble spots refuse to budge! Grrrrr! The inconvenience of it all!
We believe that Motivation, a gleaming white stallion, will gallop in from nowhere and carry us effortlessly to meaningful action—but that doesn’t happen. So there we sit, pining for that magic horse. We got it wrong. Action breeds motivation.
If we take a small step and find just a little bit of success, then we tend to want to see more success so we take further action. Several writers have discussed the action-creates-motivation dynamic.
Brad Stulberg writing in Outside Online discuses the dip in motivation during the pursuit of a goal:
“But then, when the first rough patch inevitably hits, motivation dwindles. This is when you decide to sleep in on winter mornings instead of go for a run (failed exercise plan), eat carrot cake at 11 p.m. (failed diet), or ignore your romantic partner when they tell you about their day (failed relationship goals). Even though you still want to accomplish your objectives, you may stop caring as much about them. And yet if you force yourself to show up, to take action—do the run, skip the cake, be present for your partner—and if you do this consistently, a strange thing starts to happen: Your motivation increases.”
Dr. Rubin Khoddam writes in Psychology Today explains how taking committed or valued action leads to more motivation to take more action:
“Let me give you a basic example. Have you ever felt like just staying at home and watching TV and not motivated at all to go to the gym? Yeah, me too. BUT, have you also ever noticed that you sometimes went to the gym and not only felt better about yourself but were more motivated to go back again later. That is because motivation does not precede action, action precedes motivation.
“I don’t just mean any action. I mean committed action. Valued action. What is valued action? Valued actions are actions that are consistent with your values in life. These are actions that are consistent with the type of person you want to be. I value staying healthy, so I set a goal for myself to go to exercise at least 4 days a week. My valued action is getting my butt up and going to the gym regardless of whether I am in the mood or not.”
James Clear has written an extensive article on motivation. He discusses common misconceptions about motivation:
“Motivation is often the result of action, not the cause of it. Getting started, even in very small ways, is a form of active inspiration that naturally produces momentum.
“You don’t need much motivation once you’ve started a behavior. Nearly all of the friction in a task is at the beginning. After you start, progress occurs more naturally. In other words, it is often easier to finish a task than it was to start it in the first place.
“Thus, one of the keys to getting motivated is to make it easy to start.
Clear also discusses the power of the Goldilocks Rule to stay motivated over the long haul:
“Human beings love challenges, but only if they are within the optimal zone of difficulty. Tasks that are significantly below your current abilities are boring. Tasks that are significantly beyond your current abilities are discouraging. But tasks that are right on the border of success and failure are incredibly motivating to our human brains. We want nothing more than to master a skill just beyond our current horizon.
“We can call this phenomenon The Goldilocks Rule. The Goldilocks Rule states that humans experience peak motivation when working on tasks that are right on the edge of their current abilities. Not too hard. Not too easy. Just right.”
Each of these articles mentions physcial movement as a part of motivation. Sitting still saps our motivation. Movement generates motivation. Get up. Move around. Do something that moves you forward, even if it’s just one step. The motivation will follow your action.